Introduction
Welcome to Rutherford Physio & Sports Clinic's resource about Osteoporosis.
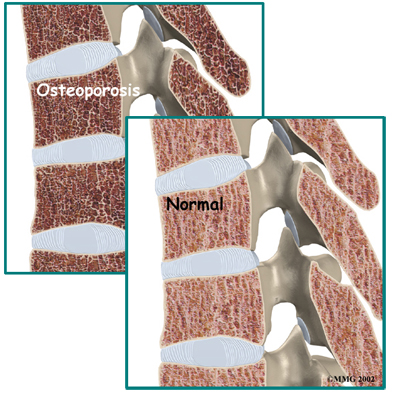
Osteoporosis is a very common disorder affecting the skeleton. In a patient with osteoporosis, the bones begin losing their minerals and support capabilities, leaving the skeleton brittle and prone to fractures.
Osteoporosis affects an estimated 75 million people in Europe, USA and Japan.
Bone fractures caused by osteoporosis have become very costly. Half of all bone fractures are related to osteoporosis. A person with a hip fracture has a 20 percent chance of dying within six months as a result of the fracture. Many people who have a fracture related to osteoporosis spend considerable time in the hospital and in rehabilitation. Often, they need to spend some time in a nursing home.
This guide will help you understand:
- what happens to your bones when you have osteoporosis
- how health care professionals diagnose the condition
- what you can do to slow or stop bone loss
- Rutherford Physio & Sports Clinic’s approach to rehabilitation
Anatomy
What happens to bones with osteoporosis?
Most people think of their bones as completely solid and unchanging. This is not true. Your bones are constantly changing as they respond to the way you use your body. As muscles get stronger, the bones underneath them also get stronger. As muscles lose strength, the bones underneath them weaken. Changes in hormone levels or the immune system can also change the way the bones degenerate and rebuild themselves.
 As a child, your bones are constantly growing and getting denser. At about age 25, you hit your peak bone mass. As an adult, you can help maintain this peak bone mass by staying active and eating a diet with enough calories, calcium, and vitamin D. Maintaining this bone mass, unfortunately, gets more difficult as we get older. Age alone makes building bone mass more difficult. In women, the loss of estrogen at menopause can cause the bones to lose density very rapidly.
As a child, your bones are constantly growing and getting denser. At about age 25, you hit your peak bone mass. As an adult, you can help maintain this peak bone mass by staying active and eating a diet with enough calories, calcium, and vitamin D. Maintaining this bone mass, unfortunately, gets more difficult as we get older. Age alone makes building bone mass more difficult. In women, the loss of estrogen at menopause can cause the bones to lose density very rapidly.
The bone cells responsible for building new bone are called osteoblasts. Stimulating the creation of osteoblasts helps your body build bone and improve bone density. The bone cells involved in degeneration of the bones are called osteoclasts. Interfering with the action of the osteoclasts can speed up bone loss.
In high-turnover osteoporosis, the osteoclasts reabsorb bone cells very quickly. The osteoblasts can't produce bone cells fast enough to keep up with the osteoclasts. The result is a loss of bone mass, particularly trabecular bone, which is the spongy bone inside vertebral bones and at the end of long bones. Postmenopausal women tend to have high-turnover osteoporosis (also known as primary type one osteoporosis). This relates to their sudden decrease in production of estrogen after menopause. Bones weakened by this type of osteoporosis are most prone to spine and wrist fractures.
In low-turnover osteoporosis, osteoclasts are working at their normal rate, but the osteoblasts aren't forming enough new bone. Aging adults tend to have low-turnover osteoporosis (also known as primary type two osteoporosis). Hip fractures are most common in people with this type of osteoporosis.
Secondary osteoporosis describes bone loss that is caused by, or secondary to, another medical problem. These other problems interfere with cell function of osteoblasts and cause over-activity of osteoclasts. Examples include imbalances in hormones, certain bone diseases and cancers, and medical conditions that result in inactivity. Some medications, especially long term use of corticosteroids, are known to cause secondary osteoporosis due to their impact on bone turnover.
Osteoporosis basically creates weak bones. When these weak bones are stressed or injured, they often fracture. Fractures most often occur in the hip or the bones of the spine (the vertebrae). They can also occur in the upper arm, wrist, knee, and ankle.
Causes
What causes osteoporosis?
Aging is one of the main risk factors for osteoporosis and osteoporotic fractures. If you are lucky enough to live a long life, you are much more likely to develop weakened bones from osteoporosis. In women, the loss of estrogen at menopause causes bone loss of up to two percent per year. Caucasian women over age 50 have a lifetime risk of fracture of about 50 percent. This figure increases with increasing age.
A number of factors contribute to or put you at risk of developing osteoporosis:
- advanced age
- female gender
- low body weight or a thin and slender build
- recent weight loss
- history of fractures
- family history of fractures
- tobacco use
- alcohol abuse
- lack of exercise
- extended use of certain medications (e.g., corticosteroids, anticonvulsants, and thyroid medicine)
- eating disorders such as anorexia or bulimia
- Asian or Caucasian race
These risk factors are just as relevant as a bone mass measurement in determining how likely you are to have a fracture. People with low bone mass but no additional risk factors often don't develop fractures. People with small amounts of bone loss but many risk factors are more likely to eventually develop fractures.
Symptoms
What does osteoporosis feel like?
Fractures caused by osteoporosis are often painful. Osteoporosis itself, however, has no symptoms. It is often called the ‘silent disease’ or ‘silent thief’ as many people don’t recognize they have it until a fracture occurs. For this reason it is especially important to get tested if you are a woman past menopause and have any of the above risk factors. Women over 65 should be tested whether or not they have other risk factors. People with other bone problems or who take drugs that weaken the bones should also be tested. An initial screening for osteoporosis is painless and easy.
Diagnosis
How do health care professionals diagnose osteoporosis?
Free osteoporosis screenings that estimate your bone density measure (BDM) are available in many drug stores and malls. Most of these screenings use a machine that scans the bone in the heel of your foot. It is a fast and simple way to get an idea of your bone density. However, this test is not entirely accurate. Due to the heel bone bearing a lot of weight in normal activity, the test may show normal bone in the heel, even though the hipbones or spine may have low bone density. If however the foot scan shows a low bone mass, you should talk to your doctor. If the scan is negative however, and you suspect you may have osteoporosis or have some of the risk factors for developing the disease that are listed above, it is still recommended that you consult with your doctor.
When visiting your doctor he or she will take a detailed medical history to help weigh your risk factors for osteoporosis. If osteoporosis is suspected or you are at risk of developing it, your doctor may also recommend more precise testing. A bone density test, or in medical terms a dual-energy X-ray absorptiometry (DEXA) test is the most common method of measuring bone mass. A DEXA test is painless and uses special X-rays of the bones of your hip and spine to show your bone mass in these areas. The bone mass is then compared to that of a healthy thirty-year-old, called a T score. If you are within one standard deviation (SD) for bone density, you have normal bone. (SD is a statistic to measure variations in how a group is distributed.) If you are between one and 2.5 SDs below ideal levels, you are considered to be osteopenic. This means you have a mild form of osteoporosis. If the bone mass is more than 2.5 SDs below ideal levels, you have osteoporosis.
Unfortunately a single DEXA scan cannot show your doctor whether your bone mass is stable, increasing, or decreasing. Your doctor may have you take certain medications that create markers in the blood or urine to show what is happening in your bones. These tests will tell your doctor if you have high-turnover or low-turnover osteoporosis.
Be aware also that DEXA scans are not perfect. Different equipment or different technicians can get somewhat different readings. If you need to have more precise data, your doctor may recommend additional types of scans or tests.
Although a DEXA scan is the most common method of measuring bone density, other tests such as ultrasound, quantitative computed tomography (CT) scans, or single-photon absorptiometry may also be used instead of or in addition to the DEXA scan to confirm the diagnosis of osteoporosis.
If bone density tests show that you have weakened bones, your doctor will need to rule out other causes for this other than osteoporosis. In some cases, problems with bone marrow or hormone levels can cause bone loss. Blood tests can show these conditions.
In other cases the bone weakening is actually from a condition called osteomalacia.
Osteomalacia involves a softening of the bones caused by a lack of vitamin D. Vitamin D in your body comes from food and sunlight. Due to a lack of sunlight, almost 10 percent of people with hip fractures in the northern parts of the world have osteomalacia rather than osteoporosis. Urine and blood tests can help rule out osteomalacia.
In some cases, your primary care physician may refer you to a doctor who specializes in osteoporosis. For instance, if you are on medication to prevent bone reasbsorption and still have significant bone loss you may need to see a specialist. Referral is also advised for patients who have recurring fractures during therapy or repeated, unexplained fractures. Your doctor will help you find the right specialist for your situation.
Treatment Options
What can be done for osteoporosis?
The goal of your treatment plan will be to prevent fractures. This is especially important if you've already suffered a fracture from osteoporosis. To prevent fractures, you need to increase your bone mass. If you have high-turnover osteoporosis, you also need to prevent rapid bone reabsorption.
You need to take several steps to increase your bone mass:
- If you smoke, quit immediately.
- If you drink alcohol, do so moderately.
- Make sure you get enough calcium and vitamin D. (Vitamin D helps your body absorb calcium.) Researchers think that increased calcium intake alone could reduce the number of fractures by 10 percent. Many people don't get enough calcium or vitamin D, especially as we age. It is difficult to get recommended levels from the food we eat, so supplements are probably necessary. Talk to your doctor about what kind of supplements to buy. Calcium comes in many forms, for example, calcium carbonate, calcium citrate, calcium phosphate, and calcium from bone meal. Some forms of calcium can be taken with any type of food, and others need to be taken with certain types of food. Taking extra calcium and vitamin D improves the effectiveness of all other treatments for osteoporosis.
- Eat enough calories to maintain a healthy weight. Being too thin increases your risk of osteoporotic fractures. Weight loss can be a cause of bone loss.
- Exercise. Your bones are constantly adjusting to the demands you put on them. Even low levels of exercise can help you maintain better bone mass. Low-impact exercises, muscle-strengthening exercises and balance training are all recommended (see section below.)
Physiotherapy
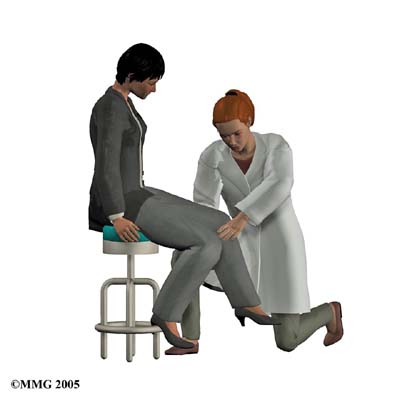
Patients with osteoporosis or those at risk of developing osteoporosis will benefit from working with a physiotherapist at Rutherford Physio & Sports Clinic.
The goals of our physiotherapy treatment is to educate you on proper posture, teach you safe ways of moving and lifting, and to provide you with exercises you can do at home to help prevent a decline in bone mass and prevent fractures. The exercises we prescribe will particularly focus on activities that help to increase the strength in your bones, as well as exercises that help to maintain or improve your balance. Optimum balance helps to decrease your risk of falling, which can easily fracture an osteoporotic bone. We will also suggest exercises for your flexibility to help decrease the stress placed on the bones by tight muscles as well as improve your overall mobility. If you have experienced a fracture from osteoporosis, physiotherapy at Rutherford Physio & Sports Clinic can also help with controlling your pain and gradually returning you back to your regular activities.
Maintaining good posture is of utmost importance if you have osteoporosis. A stooped upper spine posture, called kyphosis, is common in osteoporosis due to the wedge-like fracturing of the thoracic spine that often occurs (the front part of the vertebrae collapses leaving the posterior portion higher and the overall vertebrae appearing wedge-like.) Losing height as a result of these fractures is a common occurrence in osteoporosis. For this reason accurately measuring and recording your body height is a key part of our physiotherapy evaluation. A height measurement gives your physiotherapist an idea of how osteoporosis is affecting your bones and posture, and by comparing the recordings over a period of time it can help us track your success with treatments.
With posture exercises, the goal is to get your body lined up from head to toe, with weight going through your hips. In a healthy spine posture, the head is balanced on top of the spine rather than jutted forward which is common in osteoporosis. In people with advanced osteoporosis, the upper body is also commonly bent forward at the hips. This prevents the hip bones from getting the right amount of stress and weight through them. As a result, the bones weaken and become more prone to fracture. It is therefore important at all times to try to “be tall” which can both prevent a loss of height as well as help you regain height lost from an already fractured osteoporotic spine.
Your physiotherapist will explain ways you can put good posture into practice. This is called body mechanics, which is the way you align your body when you do your daily activities. Remember that a healthy posture is balanced with the body aligned from the head to toes. The same posture should be used when you bend forward to pick things up. Instead of rounding out your shoulders and upper back, keep the back in its healthy alignment as you bend forward at the hip joint. This keeps your back in a safe position. When bones are weakened from osteoporosis, rounding the spine forward when bending and lifting pinches the front section of the vertebrae and increases the risk of a spine fracture. This pinching is exacerbated when any weight at all is lifted in this position. Even the weight of a purse or shopping bag can add detrimental stress to an osteoporotic spine leading to a fracture. Along with maintaining proper posture, gently tightening the muscles around your core area can also help to protect the back during activities such as lifting. Your physiotherapist will educate you on how to use your core muscles to protect your spine. Rapid bending forward of the osteoporotic spine, such as that experienced when one sneezes or coughs, can be enough to cause a fracture of the osteoporotic spine. For this reason, your physiotherapist will educate you on consciously extending rather than flexing your spine during these activities.
Another motion particularly stressful for the osteoporotic spine is a twisting motion. The normal structure of bone is not designed to withstand twisting very well so combined with the weakened bone state of osteoporosis, the motion of a twist can easily cause a fracture. Although difficult to eliminate from every day life, twisting should be avoided whenever possible especially in combination with higher velocity motions such as a golf swing, tennis swing or bowling action.
Strengthening exercises for your bones are of utmost importance in maintaining the health of osteoporotic bones. As mentioned above, as your muscles get stronger, the bones underneath them also get stronger as they react to the added stress placed on them. In this way, strength training and weight-bearing activities force the bones to build mass. Your physiotherapist will prescribe some gentle weighted exercises, using either elastics or weights, for your upper and lower extremities. Using an appropriate weight is of utmost importance and your physiotherapist can educate you on how much resistance is appropriate for you. If using free weights, handling the weights is just as important as doing the exercises themselves. Never lift weights in the flexed forward posture described above, and be careful to gradually increase the resistance you use as weights that are too heavy will naturally cause your body to slip into the flexed forward posturing that is detrimental to people with osteoporosis. Performing exercises while your upper back is supported in good alignment is also recommended to avoid added stress on the thoracic spine. Exercises that incorporate flexing of the spine, such as toe touches, abdominal crunches, and dead lifts should strictly be avoided. Strengthening exercises for your upper back, however, will be encouraged by your physiotherapist in order to counteract the stooped forward posturing.
Weight bearing cardiovascular exercises such as walking outdoors or on a treadmill, gentle non-pounding forms of dance, and stair climbing are useful activities to put weight through the bones and encourage an upright posture while also improving cardiovascular health. Cycling is not a recommended activity as it does not provide the benefits of weight bearing and it also encourages the detrimental flexed forward posturing of the spine. Pool exercises are not weight bearing either so are not recommended unless severe pain from osteoporosis limits physical activity on the land in which case exercising in the pool would be acceptable and recommended. High impact activities such as running, jumping, and pounding forms of dance should be strictly avoided. Your physiotherapist at Rutherford Physio & Sports Clinic can educate you on safe cardiovascular activities specific to your interests and your physical needs.
The next part of our treatment will focus on your balance. As stated above, poor balance can lead to a fall which can easily fracture an osteoporotic bone. In some cases a fracture from a fall can be a potentially life-threatening situation. Exercises to improve your balance can be as simple as standing with your feet close together, standing on one foot, or standing with one foot in front of the other. Closing your eyes can make any of these activities even more difficult. By challenging your balance, your reaction time to unexpected situations such as tripping will improve and your likelihood of falling will decrease. The most important aspect of working your balance is ensuring that you are doing it in a safe environment. Your physiotherapist will provide you with exercises that are specific and challenging to your current level of balance. As your balance gets better, more challenging exercises will be provided. Tai chi, which is an exercise form originating in China, is another great way to improve one’s balance, and many patients benefit from practicing this on a regular basis.
The final component to our treatment at Rutherford Physio & Sports Clinic will be to provide you with some flexibility exercises. By improving and maintaining your flexibility, the stress put on your bones by tight muscles will decrease and the ability to practice good posture and body mechanics will be improved. Good flexibility also improves your mobility, which in turn improves you balance and decreases your risk of falls. Stretches for your upper back and chest in particular will be prescribed to decrease the likelihood of developing a stooped posture. Stretches for your hips, calves, and neck are also important if you have osteoporosis and will be included in your stretching regime.
Your physiotherapist will continue to compare your test results of body height, posture, strength, balance, and flexibility to see how well you are improving and to encourage you in continuing with your exercise program. Once you can safely and proficiently perform your home exercise program, regular visits to Rutherford Physio & Sports Clinic will not be required, however, we will continue to be a resource for any further questions you may have or problems you may encounter.
If you are seeing one of our physiotherapists at Rutherford Physio & Sports Clinic because you have recently had a fracture related to osteoporosis, our treatment will start with a focus on decreasing your pain. We may use hands on treatment as well as modalities such as ice, heat, ultrasound, or electrical current to assist in managing your pain. We will liaise with your doctor to determine the most appropriate time for you to begin the more advanced exercises involving strengthening, balance, and flexibility as outlined above, and will proceed with them as appropriate in order to allow you to return to your normal activities as quickly as possible.
Rutherford Physio & Sports Clinic provides services for physiotherapy in Vaughan & Richmond Hill.
Medication
Depending on your situation, your doctor may prescribe medications to slow down your body's reabsorption of bone.
Many drugs are now available for the prevention and/or treatment of osteoporosis. Finding the right drug for each patient takes into consideration the benefits and risks of the drug. These are matched against specific patient characteristics and risk factors. Ultimately, the best drug is the one most likely to be taken consistently and/or correctly by the patient.
If you are past menopause, hormone replacement therapy can be very effective. Bisphosphonates and calcitonin can also slow your body's reabsorption of bone.
Studies have shown that 80 percent of women actually build bone mass up to two percent per year while on estrogen replacement therapy. Estrogen has been shown to decrease the occurrence of fractures in the vertebrae by 50 percent and fractures in the hip by 25 percent. Fortunately studies have also shown that hormone replacement therapy can also lower rates of coronary artery disease, relieve some symptoms of menopause, and maybe even prevent or postpone Alzheimer's disease.
Hormone replacement therapy, however, worries many women. Studies have shown that it may increase the risk of breast cancer. For women with a family history of breast cancer or who have had a stroke or thrombophlebitis (blood clots), hormone replacement therapy is probably not appropriate. Other women however, should at least consider taking estrogen as its effects on osteoporosis are dramatic. Researchers estimate that, if estrogen were widely used, it could reduce all osteoporotic fractures by 50 to 75 percent.
Hormone replacement therapy must be continued to be effective, however. When a woman stops taking estrogen, she'll start to lose bone at a very fast rate again. Within seven years, her bone density will be as low as that of a woman who never took estrogen.
Doctors often prescribe calcitonin to patients with fractures. Calcitonin is a non-sex, non-steroid hormone. Calcitonin binds to osteoclasts (the bone cells that reabsorb bone) and decreases their numbers and activity levels. Calcitonin used to be given only by injection, but now it is available in a nasal spray and a rectal suppository. Nasal calcitonin is used most often for women with osteoporosis who are five years or more past menopause and unable to take other approved agents. For unknown reasons, calcitonin also seems to relieve pain.
You and your doctor need to work together to monitor the effects of calcitonin. It is a new drug, and its long-term effects and benefits are still not fully known. More than 20 percent of patients develop a resistance to calcitonin over time, and it stops working for them.
Bisphosphonates also slow reabsorption by affecting the osteoclasts. Some common bisphosphonates are Alendronate (Fosamax), Risedronate (Actonel), or Ibandronate (Boniva).
Some bisphosphonates are taken orally (pill form) on a daily basis. Others are available in weekly or monthly doses. A new injectable bisphosphonate (Zoledronate) can be given annually (once a year). Boniva comes in pill form and can also be injected once every three months. The injectable forms of this drug are used in the management of postmenopausal osteoporosis.
Studies have shown that bisphosphonates increase bone mass and prevent fractures. No one is sure how well bisphosphonates work when used for a long time however stopping the drug doesn't seem to cause the rapid bone loss that occurs when a patient stops taking estrogen. Due to the potential of side effects with these medications, you need to liaise closely with your doctor if you take them.
Some new drugs that may be used to treat osteoporosis are currently being researched. Some of these drugs, such as sodium fluoride, can be helpful in low-turnover osteoporosis. These drugs affect your osteoblasts in ways that cause them to create more bone. Sodium fluoride may be available in the near future. Another drug used for the treatment of osteoporosis is Raloxifene (Evista) which is an anti-estrogen.
Anti-estrogens are also called selective estrogen-receptor modifiers (SERMs). SERMs improve bone density and prevent fractures similar to estrogen, but without increasing the chances of hormone-related cancers. Their main benefit over hormone replacement therapy is that they do not increase the risk of breast cancer.
Raloxifene is used most often for postmenopausal women younger than 65. They must not be at risk for blood clots or have cardiovascular disease. Men may be prescribed the only anabolic agent (Teriparatide/Forteo) approved for the management of osteoporosis. Anabolic usually refers to hormones that build up muscle or bone mass. Forteo is a form of parathyroid hormone used for patients at high risk of fracture. An agent with antiresorptive effects, such as a bisphosphonate, usually follows it.
Lifestyle changes, hormone replacement therapy, exercise prescription, and recent advances in drug therapy can help you take control of your osteoporosis. You and your doctor should be able to find ways to help you prevent the debilitating fractures of osteoporosis.
Portions of this document copyright MMG, LLC.